Jane’s Beautiful Birthday Dream Grows at Ecumen of Litchfield
Jane Magnuson rarely speaks. She does not ask for much.
She is wheelchair bound. And does not like to call attention to herself.
So it was particularly difficult to figure out what to do for her birthday.
But the staff at Ecumen of Litchfield was determined to find the best possible way to celebrate.
Jane is a hospice client. This birthday is especially important.
Last year, Ecumen of Litchfield Hospice started the “EcuDreams” program to make dreams come true for clients in their last days.
Mary Buhr, the activity director, remembered that Jane loves flowers. Judy Loecken, a hospice social worker, got busy hatching a plan with the team.
Yesterday morning Judy wheeled Jane from her room. When they returned a short time later, a crowd of people were singing and showcasing Jane’s present.
It is a planter built just for her, full of flowers, to fit her room so she can wheel up to it and dig in the dirt.
Jane does not like crowds and commotion. But yesterday she smiled and nodded, clearly very pleased.
“There was not a dry eye in the room,” said Sandy Doughtery, the clinical director.
All the materials, labor, dirt and plants were donated. Dennis Gartner of Litchfield Building Center designed and built the custom planter. Marilyn Rau was there from Stockmen’s Greenhouse, which donated the dirt and flowers.
Marilyn knelt down and told Jane: “If you don’t see your favorite flowers here, just let me know and we’ll fix that.”
Everyone gathered for cupcakes.
Nicole Larson of the hospice staff knelt and fed Jane a cupcake.
Jane Magnuson turned 81 yesterday. Today she will smell the flowers.

------
POSTSCRIPT:
Activity Director Mary Buhr went back to see Jane the day after her birthday. Mary posted this account on Facebook:
" We made a great 'mess' with the dirt, and the smell of the fresh dirt filled her room. Jane was very happy --so much so she didn't want to take her planting glove off! And as I left the room, she smiled and said 'just leave me here facing my garden--I am happy now.'
Most Centenarians Feel Positive — And a Lot Younger Than They Are
UnitedHealthcare has been polling centenarians annually for the past nine years, and the studies document that the 100+ age group is overall happy, well adjusted and not burdened with regrets.
This year’s study, summarized in USA Today, finds that centenarians on average feel about 83. (Baby boomers also were surveyed this year, and on average a 65-year-old feels 55.)
Most centenarians did not expect to live to 100, and most baby boomers do not expect to reach that age. Both say that attitude and physical health are equally important to reaching 100.
Full study results are available here.
A Handy Guide to Communicating With People Who Have Dementia
Dementia gradually diminishes a person’s ability to communicate properly, requiring patience, understanding and good listening skills. The following infographic offers a few suggestions on how to overcome barriers between you and the person with dementia.

Source: Open Placement, a California firm providing seniors, families and care coordinators real-time information and tools so they can find the right senior housing and home care providers. You can find the original blog post here.
Last Week's Top 5 Blog Posts - April 28
In case you missed them, here are the blog posts our online visitors found most intereesting last week:
Ecumen's Corporate HR Team Takes Big Lessons from an Afternoon at Feed My Starving Children
Ecumen Job Openings Now on Twitter
Honor: Seven Teachings on a Life Well-Lived from Sen. Nancy Brataas and Her Daughter Anne
Thankful Family Honors Grand Village Caregivers
Ecumen Prairie Lodge: Anisah's Rich, Full Life (Video)
For more information about Ecumen or its 37 locations, please visit ecumen.org.
Honor: 7 Teachings on a Life Well-Lived from Senator Nancy Brataas and Her Daughter Anne
Anne Brataas is the daughter of pioneering Minnesota State Senator and leader Nancy Brataas. Sen. Brataas, who was the first female Minnesota state legislator elected in her own right, died last week in hospice care. For a wonderful example of "honor," we share with you her daughter's tribute entitled: As she died, Sen. Nancy Brataas posed a final question: 'Unconventional?' that was published today at MinnPost.com.
Ecumen Job Openings Now on Twitter
Ecumen’s Human Resources Department recently launched the new @Ecumen_Jobs Twitter account that highlights open positions in the company’s 37 cities in Minnesota, North Dakota, Wisconsin, Nebraska, Idaho and Tennessee. As one of the top 20 nonprofit senior services providers in the nation, Ecumen offers a wide variety of jobs along numerous career paths to more than 4,000 employees.
Positions include an array of opportunities in direct health care, such as nursing and other caregiving and therapy jobs, as well as positions in sales and marketing, accounting, human resources, social services, IT, housing management, building maintenance and housekeeping, food and dining services, and administrative support.
Jobseekers can apply online for Ecumen jobs at http://careers.ecumen.org/jobs/.
Ecumen’s Corporate HR Team Takes Big Lessons From an Afternoon at Feed My Starving Children
By Camille Gross, Ecumen E-Learning and Training Coordinator
Ecumen’s mission primarily focuses on serving older adults, but it’s great to be part of an organization that encourages us to serve all ages.
Last week the Ecumen corporate Human Resources team went on a volunteer outing to Feed My Starving Children’s site in Coon Rapids, Minn. We quickly learned how much of a difference just a little help can make in the lives of others.
We packed food shipments to Jamaica and had an experience far more enlightening than we expected.
It’s incredible to think that a few hours of volunteer work could have such an impact. Over the course of a half day’s work, we were able to pack 47 boxes of food. With each box containing 216 meals, we were able to pack over 10,000 meals. We were told that our efforts were enough to feed 166 children for an entire year. Plus we got to wear cute hairnets and taste the food.
Also, the experience brought us closer as a team. Packing food in an assembly line process, the nine people in our group became more comfortable as a team and felt a drive to become better – together. To ensure the success of the overall purpose, we had to rely on one another.
Some of us measured out the food — dried rice, soy and vegetables, along with vitamins. Others weighed and sealed packages. Others packed boxes. We quickly found ourselves in competition with other groups of volunteers — trying to see who could pack the most boxes.
It was a fun atmosphere, but we were focused on the job and driven to work as efficiently as we could. At the time we probably didn’t realize it, but looking back, this is how our department must operate every day in order to succeed. We must strive towards the same goals and trust each other to support Ecumen employees in the best way we can.
Ecumen encourages employees to collaborate and provide excellent service to the people and communities we serve— and also to volunteer outside the company to help the community at large. We got a first-hand lesson in why that is such a good idea. Here’s the bottom line on our afternoon of volunteering:
- Boxes of food packaged= 47.
- Children fed for one year=166.
- Experiencing the value of service= Priceless.
Ecumen Prairie Lodge: Anisah’s Rich, Full Life
Meet Anisah, an artist with poise, grace and an endearing approach to life. Anisah is a resident of Ecumen Prairie Lodge, a senior living community in Brooklyn Center, Minn. She has everything she wants, but her riches have nothing to do with money. Let her tell you what really matters in life.
Last Week's Top 5 Blog Posts - April 21
In case you missed them, here are the blog posts our online visitors found most interesting last week:
Thankful Family Honors Grand Village Caregivers
How to be a Good Caregiver When the Caregivee Doesn't Want Your Help
Ecumen's Christy Johnson Gets Very Serious About Fun and Games
Great Minds Gala Video: Ashley and Shannon Campbell Perform Tribute to Their Father
A Look at Alzheimer's Through the Eyes of a Young Doctor
For more information about Ecumen or its 37 locations, please visit ecumen.org.
Thankful Family Honors Grand Village Caregivers
Her phone was ringing off the hook. Roberta Alzen, the director of nursing at Ecumen-managed Grand Village in Grand Rapids, Minn., was caught off guard.
“Have you seen the paper?” the callers all wanted to know. She had not, but would quickly find out that she and the staff at Grand Village were being honored in a deeply touching way.
Prominently displayed on the editorial page of the Sunday Grand Rapids Herald Review was a letter from a grieving mother who had just lost her son.
Dottie Wilde of Grand Rapids had just said goodbye to her son, Donald. He was only 55. In 2012 he had a stroke and never fully recovered.
Now she wanted everyone in the community to know how well he had been cared for the last two years of his life at Grand Village — two very difficult years. “I was so thankful he was in such a good home and he got the best care he could have received,” Dottie wrote. “Everyone is so caring and so kind and they give such good nursing care to everyone.”
What made this appreciation so much more meaningful was Dottie’s background. “I spent 42 years in nursing myself,” she wrote, “so I feel I know what good patient care is. I feel the nursing staff not only takes care of the residents and patients but they also take care of the families of the residents.”
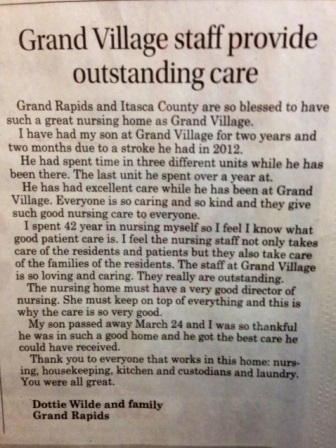 And there was special mention of Roberta, as the director of nursing. “She must keep on top of everything and this is why the care is so very good,” Dottie wrote. And she concluded: “Thank you to everyone that works in this home: nursing, housekeeping, kitchen and custodians and laundry. You were all great.”
And there was special mention of Roberta, as the director of nursing. “She must keep on top of everything and this is why the care is so very good,” Dottie wrote. And she concluded: “Thank you to everyone that works in this home: nursing, housekeeping, kitchen and custodians and laundry. You were all great.”
Roberta said everyone at Grand Village was moved by such heartfelt and public thanks. She said because Donnie was so young and had so many challenges, he was a special member of the community. Everyone got involved in his care, and he, in turn, did what he could to help take care of the older members of the community.
“We all worked as a team,” Roberta said.
In this small community, Roberta said sometimes family members of residents will recognize her on the street and give her a hug. But this is the first time she and her staff have been honored so publicly.
And it means a lot. She said everyone on the staff learned from the journey with Donnie. And then — that day when they picked up the paper — they learned just how much what they did really mattered.





